
The knee joint is formed where the thigh bone (femur) meets the shin bone (tibia). A smooth cushion of articular cartilage covers the ends of both these bones. Healthy cartilage absorbs stress and allows the bones to glide across each other smoothly. This cartilage is kept slippery by joint fluid (synovial fluid) made by the joint lining (synovial membrane). The fluid is contained in a soft tissue enclosure around the knee called the joint capsule. The ligaments give the knee stability, and the muscles power the knee and leg for movement.
The kneecap (patella) is the moveable bone on the front of the knee. It is situated within a tendon that connects the muscle on the front of the thigh (quadriceps) to the lower leg. The surface on the back of the patella is covered with articular cartilage also. It glides within a groove on the front of the femur.
Healthy articular cartilage absorbs stress and allows the bones to glide across each other smoothly, allowing pain free movement and activities. The cartilage is kept slippery by joint fluid (synovial fluid) made by the joint lining (synovial membrane). The fluid is contained in a soft tissue enclosure around the hip called the joint capsule. The ligaments and strong muscles surrounding the hip give the hip power and stability.

A healthy joint is one that bends easily. It absorbs stress and allows pain- free movement and activities. When the joint is damaged, it may lose the ability to cushion stresses placed upon it, and movement may become painful. Sometimes a damaged knee joint will swell and hurt even when you are at rest.
It is the articular cartilage that covers the ends of the bones that becomes damaged. It starts to crack and wear away. The cartilage is not able to heal itself, and the damage may keep increasing. At first, the knee may be just a little stiff, but as the bones begin to rub together you are more likely to feel pain.
A joint replacement gives the knee new surfaces, which move smoothly and less painfully. It is not the same as a healthy joint, but works well. The goal of joint replacement is to give pain relief, which may help you return to many of your activities.

This is a degenerative disease. Years of normal use can cause articular cartilage to crack and wear away. As the ends of the bones rub against each other they become rough and pitted, and eventually the cartilage may wear away altogether. This results in stiffness, pain and loss of function.
Being overweight, or having alignment problems, (e.g. bow legs or knocked knees) puts extra stress on the joint, which may speed up the damage process.
According to the World Health Organisation osteoarthritis affects half the world’s population over the age of 65. The causes are not well understood. Ageing is the factor most strongly associated with OA. Genetic factors are among the major causes.
Onset of OA can also occur as a secondary effect of injury. For example, a bad fall, blow to the knee, previous fracture, or ligamentous injury can injure the articular cartilage leading to OA.


Once your new joint has healed properly, you should look forward to some or all of the following benefits:
• Greatly reduced joint pain.
• Increased leg strength. Without knee pain you will be able to exercise more and this will help to build up the muscles around the knee.
• Improved quality of life by allowing you to do daily tasks and low-impact activities in greater comfort.
• Correction of angular leg deformity i.e. knock-knee or bow-legs.

The procedure leaves a 3-4 inch incision compared to an 8-12 inch incision for conventional total knee replacement.
• There is no dislocation of the patella (kneecap) during the procedure, which leads to less pain and a more rapid recovery.
• There is minimal blood loss.
• Most people experience less post-operative pain.
• It usually requires a shorter hospital stay.
• Faster rehabilitation and recovery.
• Most experience an increased range of motion when compared to the total knee replacement.

Not everyone wishes to have, or requires, knee joint replacement when they have damage to their articular cartilage. Some people will have different pain tolerances, and others may not wish to undertake the risks this surgery carries.
Alternatives to surgery include:
• Regular pain medication.
• Using walking aids to reduce stress on the joint.
• Weight loss to reduce stress on the joint.
• Special shoe inserts that help to cushion the joint.
• Exercises to maintain joint movement, muscle strength and help with pain relief.
• Activity modification.
Only when these measures fail to give acceptable pain relief, is a total knee replacement offered.

It is important that you should be satisfied with the result of your knee eplacement. It is said that a knee replacement that works well can give you the knee of a sixty year old.
Satisfied patients with realistic expectations:
• Follow instructions better
• Recover quicker
• Their replacement lasts longer
Satisfaction has been shown to depend on these three factors:
1. Severity of preoperative pain and stiffness. The more pain you have before the operation, the greater the relief the surgery may give.
2. Outcome of the operation. The less the operation relieves the pain the lesser the satisfaction will be.
3. Expectations before the operation. Very high expectations usually are not satisfied by knee replacement.
It is important to realise that not all your knee pain may be abolished after your surgery. Immediately after surgery, the gnawing severe pain will have gone and be replaced by surgical pain. This may last up to 6 months but should lessen over time. Pain medication may still be needed because of this.
You may experience occasional pain in your new knee after walking and other activities. The relief of this type of pain is individual, depending on the severity of preoperative deformity in your knee, on the state of your muscles, and so on.
Remember your surgeon replaced only the damaged joint surfaces but could do nothing to the muscles, ligaments and other soft tissues equally damaged by the “joint” disease.

As with all major surgical procedures, complications can occur although everything possible is done to minimise the risks. It is important you understand the following before undertaking joint replacement surgery.
• Anaesthetic risks – will be discussed with you by your Anaesthetist.
• Deep Vein Thrombosis (DVT) – “clot in the calf” – 10% risk.
• Complex Regional Pain Syndrome. (An abnormal pain reaction to any surgery, which may need prolonged physiotherapy or pain clinic).
• Infection – this can occur while you are still in hospital, or may not become apparent for months or even years later. Our hospital constantly audits the infection rate. If your knee replacement gets infected, part or all of it may need to be removed. It is usually possible to have a good result from the revision surgery. If this fails it can lead to having the knee fused so that it doesn’t bend 1:1000 or, at worst, an amputation through the thigh 1:3000.
• Stiffness – occasionally the ability to bend the knee does not return to normal. If your knee is still stiff and not improving 3 months after surgery, it may mean a return to theatre to regain movement when you are under anaesthetic.
• Loosening – This is the major reason replacement joints fail. A loose prosthesis is a problem because it causes pain. Eventually it will lead to a further operation to revise the joint.
• Damage to nearby blood vessels and nerves are very rare but may sometimes happen.
• Death 1% - commonest causes are blood clots on the lungs or heart problems.

The decision to proceed with surgery should be made jointly by you, the patient, and your surgeon. This decision should only be made after you feel that you understand both the benefits and the risks involved with this surgery and have had chance to ask questions.
If you decide to proceed, you will have a general health check at the time of your clinic appointment, and be expected to attend a pre-operative clinic when the time for your surgery is near. At this time, you will be assessed to determine your fitness for anaesthesia, blood tests will be done, and an ECG to check your heart. There will also be another opportunity to ask questions.
Once you are listed for surgery, make sure that you have any tooth or gum problems treated before your operation. If you don’t, there is a risk that germs in your mouth could enter the blood stream and infect your new joint. If for any reason you change your mind about surgery, it is not a problem, but it is better to let us know in advance of your surgery date, so that we can allocate another patient in your place.

What do I have to do before my surgery?
• You will receive a letter with the details of your admission 3-6 weeks prior to your surgery. You may be admitted the day before, or on the same day as your surgery.
• For 72 hours prior to your admission, avoid alcoholic drinks and drink 3-4 litres of fluid e.g. tea, water every day.
• If you smoke, try to stop prior to your admission to hospital.
• Follow the advice given by the pre-operative assessment nurse about your medicines, including herbal remedies.
• If you live alone, it is advisable to stock up your freezer with easy to cook meals for when you return home. See if you can make arrangements for someone to help with buying fresh food and help with cleaning and laundry.
• Get a neighbour, friend or relative to look after your house.
• If you develop a cough, cold, chest or skin infection, or an infected in-growing toenail, please let us know, as it may be necessary to postpone surgery until you have recovered.
What will happen on admission to hospital?
• The anaesthetist will see you. They will discuss the anaesthetic with you and your pain management after the operation. You can also discuss any worries you may have.
• If you did not see a doctor at your pre-operative visit, the doctor will see you, explain the operation again and you will sign the consent form and go for an x-ray if necessary.
• The doctor will also mark your appropriate leg with a felt tip.
What will happen on the day of my operation?
• You will not be able to eat or drink (including water, sweets) for a minimum of 6 hours before your surgery.
• You will be asked to take a bath or a shower before the operation.
• You will be taken to theatre, on a bed or in a wheelchair, by a nurse.
• In the anaesthetic room the anaesthetist will give you your anaesthetic.
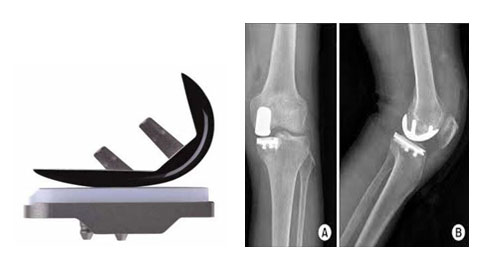
The artificial knee The surgeon makes the decision regarding which prosthesis to use, based on your age, your lifestyle and the surgeon’s experience.The operation To begin the procedure, your surgeon makes an incision on the front of the knee to allow access to the joint. Once the knee joint is opened, a special positioning device (cutting guide) is placed on the end of the femur. With the help of the cutting guide, your surgeon cuts several pieces of bone from the end of the femur.
The artificial knee will replace these worn surfaces with a metal surface. Next, the surface of the tibia is prepared. Another type of cutting guide is used to cut the tibia in the correct alignment.
The metal or oxinium femoral component is then placed on the femur and secured.
The tibial component (bottom portion) replaces the top surface of the lower bone the tibia, and is made of titanium.
A high-density polyethylene spacer sits between them.
The cemented prosthesis is held in place by acrylic cement that attaches the metal to the bone.
Finally, the soft tissues are sewn back together and staples or sutures are used to hold the skin incision together.
After the operation, you will wake up in the recovery room in your bed.
The following may be attached to you:
• An oxygen mask - take occasional deep breaths.
• A drip in your arm.
• A blood transfusion may rarely be necessary.
• Catheter: a tube into your bladder.
• Bulky bandage from mid thigh to upper calf.
• Foot pumps which aid circulation and help to prevent blood clots forming.
• Medications may be administered to prevent blood clots.
• Pain relief system- remember, we can only help you with pain if you tell us how the pain is.
• Your leg may be elevated on pillows.
Once you are stable in recovery, you will be taken back to the ward. That evening the nurses will check you regularly. You can have visitors but you are likely to be tired and drowsy, so try and keep them to a mini
mum.
What will happen on the days following my surgery?
Day of operation
• You may be able to start some exercise, under the supervision of the physiotherapist. You may be given breathing exercises to help your chest after the anaesthetic, and they also help circulation. Moving both your feet and ankles up and down and in circles quite vigorously also helps circulation.
• If you feel well enough, you may be able to sit out of bed, with assistance.
• When lying in bed, or sat in the chair, keep moving feet and ankles up and down to help with your circulation.
Day one
• You will be assisted with a full bed bath.
• You will have a blood test.
• The drip will be taken down if you are drinking well, not feeling sick and do not need a blood transfusion.
• The dressings will be removed.
• You will be able to start or continue some exercise, under the supervision of the physiotherapist (as detailed above on ‘day of operation’).
• You will start to walk, usually with a Zimmer frame at first, and gradually progress to crutches.
• The physiotherapist or assistant will see you 1 or 2 times a day.
• The physiotherapist will instruct you on exercises to get your knee bending. Should this prove difficult, then a continuous passive motion (CPM) machine may be used. This bends the knee for you and can be left on for long periods. The aim is to get the knee to bend to at least 90 degrees. It does not replace the need for you to continue with your own exercises. The knee will feel tight and sore to bend but will get easier with time.
• The knee will still be sore, so keep taking pain relief medication as needed.
• If the knee is swollen, ice will be offered, do not keep this on for more than 15-20 minutes. You may ask for ice at any time.
• Elevating the leg on a stool or bed will also help reduce swelling.
• The catheter in your bladder, if you have needed one, will be removed when you are able to walk to the toilet.
Day two and onwards
• You will have a check x-ray taken, when it is comfortable to do so.
• Your walking will continue to improve as you become more confident.
• Knee exercises will continue.
• An occupational therapist may see you to give advice on washing and dressing. If you live alone, they may check that you can manage to get your meals safely. They can also advise you if you need help with shopping or cleaning. Some people can have problems sitting if chairs and toilets are too low. The occupational therapist can arrange any necessary equipment to alter the height of these things.
• When you are safe on your crutches, the physiotherapists will show you the correct way to negotiate stairs (if appropriate).

You will be allowed to go home when your knee is bending well, and your consultant is happy with your progress. You will also need to be safe on your crutches, be able to negotiate stairs, manage to get off a chair, toilet and bed, and generally be able to look after yourself at home if necessary.
Most people leave hospital 2-3 nights following their surgery. If there are any postoperative complications, then you may need to stay longer. You can travel home in a car. An ambulance is only arranged in special circumstances.

The decision to proceed with surgery should be made jointly by you, the patient, and your surgeon. This decision should only be made after you feel that you understand both the benefits and the risks involved with this surgery and have had chance to ask questions.
If you decide to proceed, you will have a general health check at the time of your clinic appointment, and be expected to attend a pre-operative clinic when the time for your surgery is near. At this time, you will be assessed to determine your fitness for anaesthesia, blood tests will be done, and an ECG to check your heart. There will also be another opportunity to ask questions.
Once you are listed for surgery, make sure that you have any tooth or gum problems treated before your operation. If you don’t, there is a risk that germs in your mouth could enter the blood stream and infect your new joint. If for any reason you change your mind about surgery, it is not a problem, but it is better to let us know in advance of your surgery date, so that we can allocate another patient in your place.

Continue with all your exercises and keep progressing your walking. You will be given a physiotherapy outpatient appointment usually within a week of discharge from hospital. How long and frequently you will attend depends on your progress, but appointments are usually once a week. Transport can only be arranged if you have difficulty walking, and it is impossible for you to make your own arrangements to travel in. The district nurse will come to your home, 10-14 days after your operation, to remove stitches or clips from your wound. Some surgeons use sutures that dissolve, so this is not always necessary.
You will attend the outpatient clinic to see the doctor or arthroplasty nurse 6-12 weeks after your surgery.
Do not drive until you can safely do so (please check with your insurance company). Usually at the 6-week stage, once you have completed a simulated emergency stop in your parked car, it will be safe to drive.
This is an operation that requires hard work and determination. Your knee will be sore at times and to get the knee bending and the muscles working again will be hard work, which only you will be able to do.
Remember, every patient and every joint is different, and that this booklet is only meant as a guide as to what may happen during your hospital stay. Don’t worry if some days your knee is more stiff, swollen or painful than others, it will get better.

When you return home, keep your leg elevated for the majority of the time when you are resting, to help with the reduction of swelling. It is very normal for your leg to swell and this can take many weeks to get better.
If your knee becomes more swollen and warm it may be worth using ice to reduce your symptoms. To do this, make sure the ice is in a sealed bag, and then wrapped in a damp towel. Alternatively a bag of frozen peas wrapped in a damp towel may be used. Apply the ice for no longer than 10 minutes at any one time. You can use ice every hour if necessary.
Make sure you continue to do your exercises at least 2-3 times a day. Gradually increase the distance you walk over the coming days and weeks.
Avoid standing for long periods, as this will be uncomfortable and lead to more swelling in the knee joint. Do not twist your knee, as can happen when you turn your body without moving your feet.
Skin care
Once the wound has healed; you can massage the scar and surrounding area with a non-perfumed moisturising cream or oil. This helps to keep the skin supple and mobile, which can make the knee easier to bend. Please ask your therapist if you are unsure when or how to do this. If you expose your knee to the sun, make sure you apply a sun block or high factor sun cream to the scar, as initially it is very sensitive and can burn easily.
Remember to let your dentist know that you have had a joint replacement. The dentist may need to give you antibiotics following certain dental procedures to prevent infection.
Please seek advice if you experience any of the following
• The wound bleeds or discharges continuously.
• You feel feverish, shivery, have a temperature or feel sick.
• Your knee becomes very hot and red (It is normal for the wound to feel warm to touch).
• Increased pain not helped by medication or rest.
• Increased painful swelling not helped by ice and elevation.
• Increased pain in the calf muscle.
• Sudden onset of shortness of breath and pain when you take a breath in.
Goals to aim for
The following are general goals. You may find you achieve most or none of these, but it is important to remember every person is an individual and you will progress at your own rate. Everyone’s joint and surrounding tissues are also different at the time of surgery so try and avoid comparing your progress to that of others you see during your rehabilitation.
• To regain 90 degrees of knee bend by 1 week post operatively – ideally prior to discharge from hospital.
• To be able to get the knee fully straight within 2 weeks.
• Be able to walk without walking aids between 6-12 weeks.
• Back to driving at the earliest 6 weeks.
• Be able to climb stairs normally 3-4 months.
• If your knee is your only painful joint, you should be able to stop your pain relief by 6-12 weeks.