
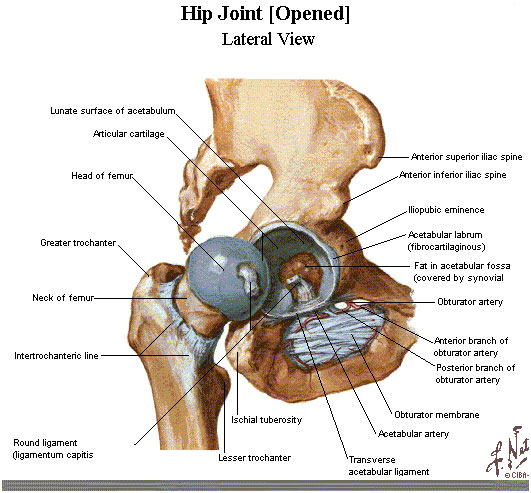
The hip is a ball and socket joint where the head of the femur sits in the cup-like acetabulum. A smooth cushion of articular cartilage covers the end of both these bones. The thick muscles of the buttock at the back, and the muscles of the thigh at the front surround the hip.
Healthy articular cartilage absorbs stress and allows the bones to glide across each other smoothly, allowing pain free movement and activities. The cartilage is kept slippery by joint fluid (synovial fluid) made by the joint lining (synovial membrane).
The fluid is contained in a soft tissue enclosure around the hip called the joint capsule. The ligaments and strong muscles surrounding the hip give the hip power and stability.

This is an inflammatory joint disease that can affect many joints within the body. It can cause swelling and heat in the joint lining. As the disease progresses it destroys the articular cartilage and eventually the bone itself is affected. Joints are usually painful, hot, swollen and stiff.

This is a degenerative disease and is often referred to as wear and tear arthritis. Years of normal use can cause the cartilage to crack and wear away and it is not able to heal itself. As the ends of the bones rub against each other, they become rough and pitted and eventually the cartilage may wear away altogether. Small outgrowths of bone spurs, called osteophytes, may form around the joint. At first the hip may be stiff, but as the bones begin to rub together you are more likely to feel increasing pain. The onset of osteoarthritis can occur from previous injury to the hip. Cartilage injuries, infection or bleeding within the joint can also damage the joint surface of the hip. According to the World Health Organisation osteoarthritis affects half of the world’s population over the age of 65. The causes are not well understood. Ageing and genetic factors are among the major causes associated with OA.


Not everyone wishes to have, or requires, a hip replacement when they have damaged their articular cartilage. Some people will have different pain tolerances and others may not wish to undertake the risks this surgery carries. Others choose to accept and live with the pain they have. Alternatives to surgery include:
• Regular pain medication.
• Using walking aids to relieve any stress on the joint.
• Weight loss to reduce the stress on the joint.
• Exercises to maintain joint movement, muscle strength and help pain relief.
• Adaptations and modifications to furniture, for example, raising the height of an armchair, bed, or using a raised toilet seat.
• Changing activities you do to reduce pain.
Only when the above measures fail to give acceptable pain relief, will a Total Hip Replacement be offered to you.

Once your new joint replacement has healed properly you should look forward to some, or all, of the following benefits.
• Greatly reduced joint pain
• Correction of deformity, for example, unequal leg length.
• Improved quality of life by allowing you to do daily activities in greater comfort.

It is important to realise that not all your hip pain may be abolished after your surgery. Immediately after surgery, the gnawing severe pain will have gone and be replaced by surgical pain. This may last up to 6-12 weeks but should lessen over time. Pain medication may still be needed because of this. You may experience occasional pain in your new hip after walking and other activities. The relief of this type of pain is individual, depending on the severity of any pre-operative deformity in your hip, on the state of your muscles, and so on. Remember your surgeon replaced only the damaged joint surfaces but could do nothing to the muscles, ligaments and other soft tissues equally damaged by the “joint” disease.
Once your new joint replacement has healed properly you should look forward to some, or all, of the following benefits.
• Greatly reduced joint pain
• Correction of deformity, for example, unequal leg length.
• Improved quality of life by allowing you to do daily activities in greater comfort.

Total hip replacement is successful in nine out of ten people. As with all major surgical procedures complications can occur, although everything possible is done to minimise the risks. It is important that you understand the following before undertaking your joint replacement surgery. This is not intended to be a complete list of all the possible complications, but these are the most common:
• Anaesthetic risks - will be discussed with you by your anaesthetist.
• Between 10 - 30 in a 100 chance of Deep vein thrombosis (DVT) - a blood clot in the calf despite preventative measures.
• 1 in a 100 chance of Pulmonary Embolism – blood clot in the lungs.
• Less than 1 in a 100 chance of infection. This can occur whilst you are still in hospital. Others may not become apparent for months or even years after the surgery. If your hip replacement gets infected, part or all of it may need to be removed. It is usually possible to have a good result from revision surgery. If this fails it can lead to having the hip replacement removed and replacing it with a scar tissue ‘joint’. (Excision Arthroplasty). This is the way hip osteoarthritis was treated before hip replacement was invented. With a stick and a shoe raise most people would eventually be able to walk comfortably.
• Infection can spread from other areas. Your surgeon may want to make sure that you take antibiotics if you need surgical procedures on your bladder or bowel. It is important to let your dentist know that you have had a joint replacement, as some dental procedures may require you to take antibiotics to reduce the risk of germs spreading to your joint replacement.
• Loosening – This is a major reason replacement joints fail. A loose joint replacement causes pain, and eventually it will need a further operation to revise the joint.
• Between 4-8 in a 100 chance of dislocation in the first year. Just like your real hip, an artificial hip can dislocate if the ball comes out of the socket. There is a greater risk in the first 12 weeks after surgery, before the tissues around the hip have fully healed, but there is always a risk. A hip that dislocates frequently may need revision surgery to make it more stable. The occupational therapist and physiotherapist will instruct you very carefully how to avoid activities and positions, which may cause the hip to dislocate.
• Damage to nearby blood vessels and nerves is very rare but may sometimes happen.
• Less than 1 in a 100 chance of fractures to the thigh bone. This can occur during surgery.
• You may sometimes find your leg is a little longer or shorter than it was before your operation and a shoe raise may be required.
• 1 in a 100 chance of death. The commonest causes are blood clots on the lungs or heart problems.

What happens before my admission to hospital?
• You will receive a letter with the details of your admission, usually within a month of surgery, but this may occasionally be less. Usually you will be admitted on the day before your surgery, but in some cases the day of your surgery.
• For 72 hours prior to admission, avoid alcoholic drinks, and drink 3-4 litres of fluid, for example, water, tea every day.
• If you smoke, try to stop prior to your admission to hospital.
• Follow the advice given by the pre-operative assessment nurse about your medicines, including herbal remedies. Herbal remedies need to be stopped 2 weeks before surgery.
• If you live alone, stock up your freezer with easy to cook meals for when you return home. See if you can make arrangements for someone to buy fresh food and help with cleaning and laundry.
• Get a relative, friend or neighbour to look after your house.
• If you develop a cough, cold, chest or skin infection, or infected in-growing toenail, please let us know, as it may be necessary to postpone surgery until you have recovered.
• Please pack your helping hand, long handled shoe-horn and sock aid if you have been supplied with them. The occupational therapist (OT) will show you how to use them whilst you are in hospital.
What will happen on admission to hospital?
• The anaesthetist will see you. They will discuss the anaesthetic with you and your pain management after the operation. You can discuss any worries you may have.
• If you did not see a doctor at your pre-operative visit, the doctor will see you, explain the operation again, and you will countersign your consent form. You may go for an x-ray if necessary.
• The doctor will also mark your hip for operation with a felt tip pen.
What will happen on the day of my operation?
• You will not be able to eat or drink (including water, sweets) for 6 hours before your surgery.
• You will be asked to take a bath or a shower before the operation.
You will be taken to theatre by a nurse on a bed or in a wheelchair. In the anaesthetic room the anaesthetist will administer the anaesthetic to you.