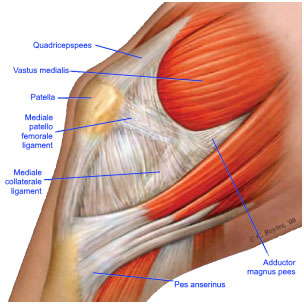
The MPFL is a ligament on the inside of your knee which attaches your kneecap (patella) to your thigh bone (femur). This ligament prevents the knee from moving abnormally and dislocating. The ligament is usually damaged when the kneecap dislocates.
When you dislocate your kneecap, it moves to the outside (lateral aspect) of your knee joint which can cause the MPFL to stretch and tear.
After the first dislocation, the MPFL will usually heal in a brace after 6 weeks, however, if it doesn’t (about 10% of cases), it leads to recurrent dislocation.

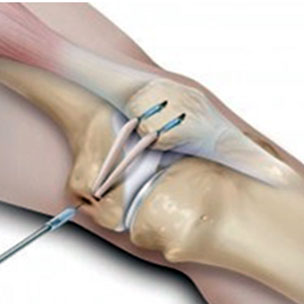
The operation is done under a general anaesthetic (when you are asleep) to allow you to fully relax. It is done by using a minimally invasive technique which means scarring and the risk of infection is as less as possible.
Four small incisions (cuts) are made around the knee to access the joint and a small portion of the hamstring is then passed through small drill holes in the knee cap. The other end is then inserted it into the inner aspect of the thigh bone using a plastic screw to hold it in place. This stabilises the movement of the knee cap.The procedure takes around one hour.
Benefits of Surgery
Success rates are high in terms of improving function and reducing instability of the patella:
• Improved knee stability with reduced chance of patella dislocation
• Improved function/mobility
• Reduced pain
• It may take up to 12 months for a full recovery and return to sport
Some people will have persisting symptoms depending on the anatomy of their knee joint, any damage already done to the bone surface and how well they engage with their post op rehabilitation in Physiotherapy.

It is likely that your pain will be well controlled immediately post-operative as local anaesthetic is usually placed into the joint during the procedure. It is therefore sensible to take some regular pain relief so that when the local anaesthetic wears off you remain comfortable. It is important your pain is under control before you leave hospital.
Should you experience any increase in pain and swelling not relieved by elevation and rest, or any pain in the calf, please contact your consultant.
Ice
Ice can be very useful to help manage swelling and pain. You need to be careful with it’s use to ensure you do not damage your skin. We suggest you follow the precautions below:
• You should ensure that the area to be treated is sensitive to temperature by placing a cold and then a warm object against it and making sure you can tell the difference
• Use crushed ice, gel packs or frozen peas as an ice pack but always ensure that there are two layers of towel between your skin and the ice pack
• Check your skin after 10 minutes, it is likely to be red but should not be white or blue. If you are concerned then remove the ice pack immediately. If your skin is frail or you have poor circulation you should check after five minutes. If there is no adverse reaction then the pack can be applied for a total of 20 minutes
Ice packs are most effective when applied for 10-20 minutes every three-four hours.
If you feel pain at any stage, always remove the ice pack and check the skin for signs of loss of circulation e.g. white/purple/blue or very cold skin. Ice packs used incorrectly can cause ice burns.
Swelling
Your knee may swell for a couple of months or even longer after the surgery. It is normal to have occasional swelling for up to a year. This is a normal part of healing but if it becomes excessive this can lead to increased pain and slower return to activities. To prevent this, sit with your foot elevated higher than your hip whenever possible and pace your activities.
If at any time you notice any discharge, smell, irritation, or redness around the wounds/dressings, you must contact your consultant as this could be a sign of an infection.
Brace
For the next 6 weeks, you are required to wear a brace that allows your knee to move from 0 to 90 degrees.
The brace will prevent any unwanted movement at your knee joint whilst recovering from surgery. A physiotherapist will visit you to ensure that the brace is fitted appropriately. They will also teach you how to apply and take off the brace. It is vital that you have the brace fitted properly before getting up after your operation, and that you are confident to use it when you are home.
Mobility
You are able to mobilise fully weight bearing as tolerated unless told otherwise. This means you can put as much weight through the leg as you are able to following your surgery. This will help the healing process. You will need to walk with crutches initially whilst you are recovering to make sure you have a correct walking pattern and help your balance. Once you have a good walking pattern you can discard the crutches and your Physiotherapist will guide you on this.
You will be able to leave hospital when you can bend your knee 90° and completely straighten your knee. The Physiotherapist on the ward will help you with this, and make sure you are safe mobilising including on the stairs before discharge.